The Pains of Increased Disinfection Protocols on Wall Coatings in Healthcare

The COVID-19 pandemic was brought on by the spread of the SARS-CoV-2 virus across the world. COVID-19 presents its own set of challenges and pains for hospitals and healthcare professionals because of its ability to spread on surfaces in healthcare facilities. However, this recent acute issue serves to aggravate an already existing chronic condition in which a host of microorganisms, such as viruses (i.e., influenza and noroviruses), bacteria (i.e., E. coli, C. difficile, MRSA) and other microbial pathogens, cause such significant risks to patient health that healthcare organizations have dedicated personnel, procedures and budgets targeted at controlling or eradicating healthcare-associated infections (HAIs), also known as hospital-acquired infections. Because this is an ongoing battle, national healthcare organizations, such as the Centers for Disease Control and Prevention (CDC), The Joint Commission (TJC) and Environmental Protection Agency (EPA), have developed and routinely update strict guidelines for addressing HAIs in healthcare facilities. These detailed protocols have been extremely effective in controlling infections over the years. However, some guidelines, including disinfection of architectural surfaces with harsh chemicals and techniques, exact a toll on some areas of the healthcare infrastructure. One observation of these heightened actions is the accelerated degradation of painted wall surfaces in healthcare facility rooms that are considered higher risk due to the activities performed in the area and the need for increased hygiene precautions.
For hospital administrators, facility managers and members of the architectural community who are concerned with meeting current CDC and TJC guidelines and heightened COVID-19 precautions in the EPA’s Emerging Viral Pathogen Policy, without sacrificing aesthetics and durability, there are architectural coating technologies for targeted hospital environments that require a higher frequency of cleaning with harsher disinfectants. This novel coating technology offers improved durability and resistance to harsh cleaners and disinfectants without sacrificing appearance. First, we must understand the symptoms of current and newer disinfection requirements, the chemicals and procedures involved, the magnitude and spread of the problem, the diagnosis process, and the deleterious effects of not treating the problem. Then, we can review and compare the possible prescriptive treatments, benchmark testing methods and results, and infrastructure “recovery” examples related to this topic.
Observing the Symptoms and Aggravating Conditions
HAIs occur in all care settings, including hospitals, surgical centers, ambulatory clinics and long-term care facilities, such as nursing homes and rehabilitation facilities. HAI has become a major threat to human life over the past several decades, with an increased volume of patients requiring medical attention and the ongoing resistance of certain microbes to traditional antibiotics. For example, in American hospitals alone, the CDC tabulates HAIs yearly based on required data collected by hospitals estimating that HAIs account for 1.7 million infections and 99,000 associated deaths annually. Patients who acquire infections from surgery spend, on average, an additional six-and-a-half days in the hospital, are five times more likely to be readmitted after discharge and twice as likely to die. Surgical infections are believed to account for up to $10 billion in healthcare expenditures annually. 1
The COVID-19 pandemic has increased the need for and frequency of stringent disinfection. In 2008, the CDC revised protocols known as the Guideline for Disinfection and Sterilization in Healthcare Facilities. Some changes affected the way critical areas, such as emergency, operating and procedure rooms, are disinfected between each patient use and during terminal cleaning. 2 In 2020, the EPA’s Emerging Viral Pathogen Policy was issued to provide specific guidance related to COVID-19. For past reasons and new challenges, there are three primary aggravating conditions that traditional wall paints face in the healthcare environment:
- Abrasion from existing disinfection guidelines;
- Paint surface degradation from disinfection chemicals; and
- Newer disinfection methods and devices.
Cleaning horizontal and vertical surfaces more often subjects the existing wall paint to increased abrasion, which it may not have been exposed to in the past. This increased abrasion can be caused by several reasons. First, more frequent use of the area can affect the wall coating’s durability. However, certain areas of the walls near tray tables and other auxiliary equipment are routinely cleaned by hospital environmental services personnel when biological contaminants may have transferred due to touch or splatter. These areas can be cleaned using commonly available pre-treated disposable wipes wetted with a 1:10 sodium hypochlorite (bleach) solution for effective disinfecting against infectious organisms. Repeatedly wiping the wall surface with a fibrous disposable material along with the strong concentration of bleach can cause a traditional wall paint to break down over time. This poses a hygiene issue since the loss of the continuous paint film exposes the porous drywall surface, which can allow absorption of biological contaminants and make the disinfection process more difficult. An additional aggravating condition can be the use of a lower-sheen wall paint that was selected for aesthetic reasons. The healthcare community prefers a warm, welcoming environment for patients in an often stressful situation. These types of finishes typically do not resist scrubbing and abrasion as well as their high-gloss counterparts. To marginally extend longevity, hospital facility managers and coating formulators often limit their design palette of acrylic latex paints to gloss or semi-gloss finishes in critical areas.
However, abrasion is not the only aggravating condition of wall paint failure. The regulations on disinfecting chemicals and cleaners and their strength have challenged the chemical resistance inherent in traditional architectural coatings. Due to COVID-19, hospitals and healthcare facilities have instituted even more aggressive cleaning regimes on vertical wall and horizontal floor areas. Recently, the EPA created List N, which defines the products containing the specific disinfectant chemicals and contact times to control the virus. The contact time, which is the amount of time the surface should be visibly wet, must be considered since these times vary by product and chemistry. This point is often overlooked since most people equate cleaning a surface to wiping their kitchen table after a meal. However, in the healthcare sector, hospital personnel are well-trained in the need to have the correct contact or dwell time on the surface in order to achieve adequate and thorough disinfection. Table 1 shows an abbreviated, generic list of active ingredients and contact times from List N.
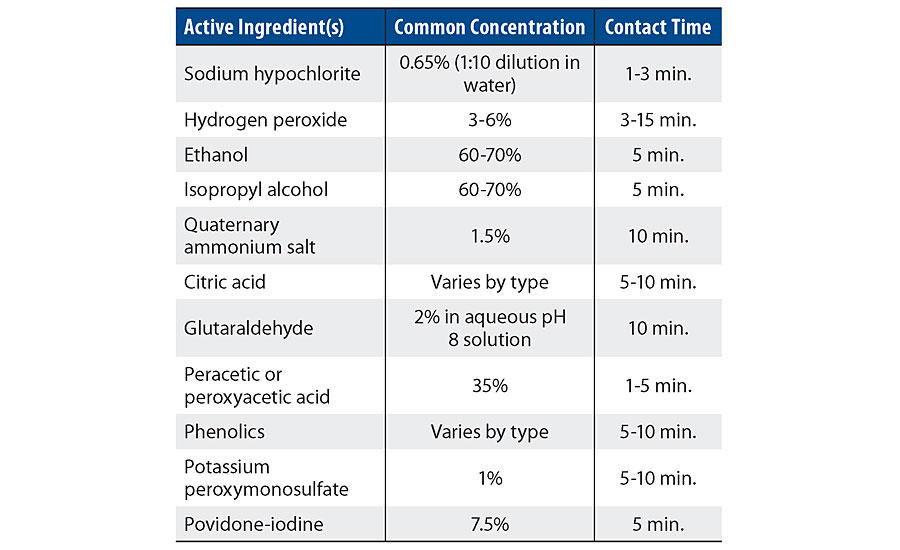
Many of the products deemed effective for destroying the SARS-CoV-2 virus are a mixture of several different chemicals to increase their efficacy, and can be even more challenging considering the chemical resistance of a wall paint or coating.
Another aggravating condition for the long-term performance of architectural wall paints is the advent of several methods and technologies for disinfecting and sterilizing critical areas of the healthcare environment. Two methods are particularly relevant:
- Surface disinfection treatment by airless spray application: These spray units are specifically outfitted with the correct materials of construction to resist the often corrosive disinfection chemicals. The equipment is used to apply a film of EPA List N chemicals on walls, furniture and other equipment as prescribed by the relevant guidelines. This method efficiently covers large areas in a short period with the correct wet film thickness to adhere to the EPA’s contact times. However, a disadvantage can be repeated secondary exposure on nearby wall surfaces from the overspray, which adds to the primary chemical exposure on wall surfaces and accelerates possible degradation.
- Automated systems, such as vaporized hydrogen peroxide, ozone mist systems and UV-C light units: Newer disinfection and sterilization methods are centered on reduced chemical exposure of the hospital environmental services personnel or more effective disinfection methods that preclude the presence of personnel. In the first case, an automated system fogs or mists the room and all the contents with a predetermined concentration of a product, such as hydrogen peroxide or ozone. In the latter case, high-energy UV-C light unit systems are used to disinfect or sterilize surfaces in critical care rooms. In both examples, exposure to traditional wall coatings can cause chemical attack, add to the degradation load on the wall surface and, in the case of the UV-C method, cause color changes of certain wall coating types.
With these aggravating conditions, in addition to the healthcare community’s aesthetic preferences, it was important to determine the top pains and gather a statistical weighting of importance of them in relation to each other via in-market interviews conducted with architects, consultants and hospital facility owners. Three main attributes for a healthcare wall coating were shared repeatedly and became the most important attributes to consider in new coating technology development: low odor, durability and price. 3 These weighted attributes are depicted in Figure 1.
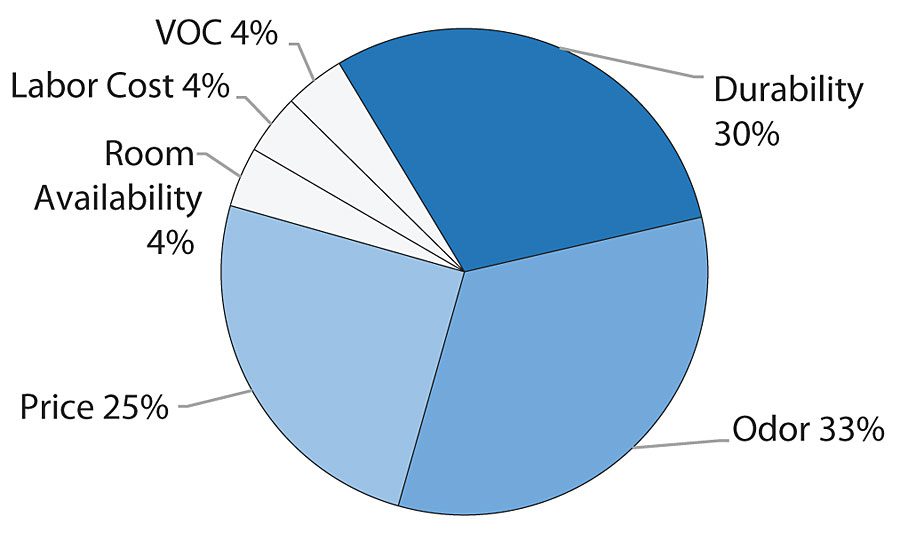
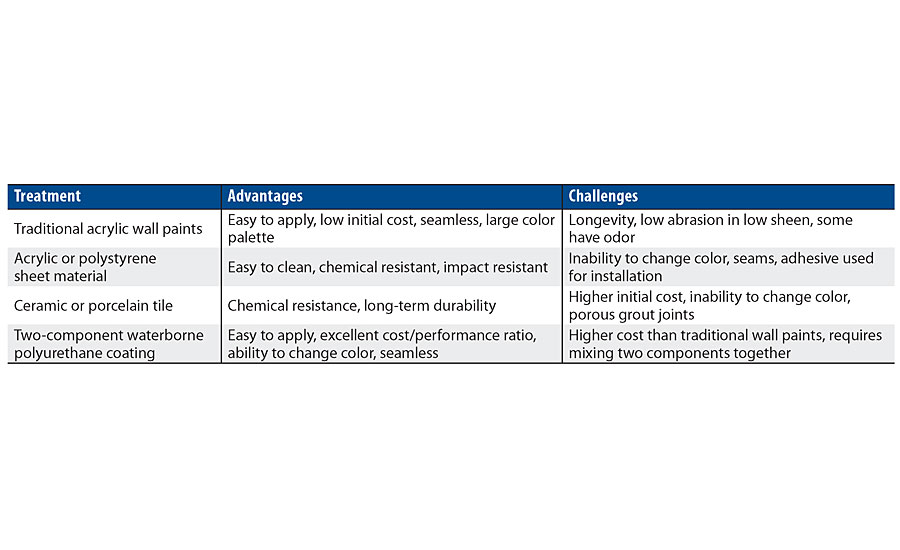
Based on these desired attributes, a study was initiated to determine a performance baseline for the common hospital architectural paints and alternative coatings (Table 2). Then, a waterborne polyurethane option was developed and compared to the benchmarking data to note any improvements in key desirable traits. A waterborne polyurethane coating was selected due to the low odor, durability and ability to adjust gloss demonstrated in other adjacent market areas. 4
Prescription for the Problem
Current and newer disinfection chemicals and procedures were researched, and a list of the most common disinfection chemicals was generated and sourced for testing. Additionally, based on the discussions with hospital facility managers and recommendations from their paint manufacturers in these targeted environments, several architectural waterborne acrylic latex wall paints were purchased and applied to wallboard samples following the manufacturer’s directions. Also, four waterborne epoxy coatings were included in the testing based on an internet search for “higher performance” and/or “healthcare” wall coatings, and the subsequent recommendation from two coating supplier web pages on this topic.
Several two-component (2K) waterborne polyurethane coating technologies were also considered for use in this environment due to their desirable physical traits, including:
- Extreme resistance to targeted harsh disinfection chemicals, such as bleach, quaternary ammonium salts, hydrogen peroxide and others.
- Excellent resistance to abrasion from heightened scrubbing and cleaning protocols.
- Near-zero volatile organic compound (VOC) formulas with excellent abrasion and chemical resistance.
- Minimal odor when applied in adjacent hospital environments.
- Multiple high-property sheen levels, including gloss, semi-gloss, eggshell and matte.
Guide formulas were prepared using 2K waterborne polyurethane resins and water-dispersible aliphatic hardeners from Covestro, along with the necessary pigments and additives. Two gloss levels were tested. These targeted gloss levels were achieved not by incorporating significant quantities of matting aids (i.e., silica flattening agents), but by the resins employed in the formula. A water-dispersible aliphatic hardener was used as the crosslinker with a ratio of 3:1. The pigmented guide formula coatings, coated over a wall primer, were applied at approximately 4-6 wet mils with a dry mil thickness of approximately 2-3 mils per coat. Dry times for the coatings ranged from 30 min for the matte formulas to approximately 1 hr for the higher gloss formula. The trend was noted that as the formulas were made to be less glossy, the dry time was reduced. For the purpose of the following testing, the 2K waterborne polyurethane with the low gloss was used since it represented the healthcare community’s aesthetic desires and the worst case scenario in regard to durability for the facility owner.
Testing the Remedy
Scrub and Stain Resistance
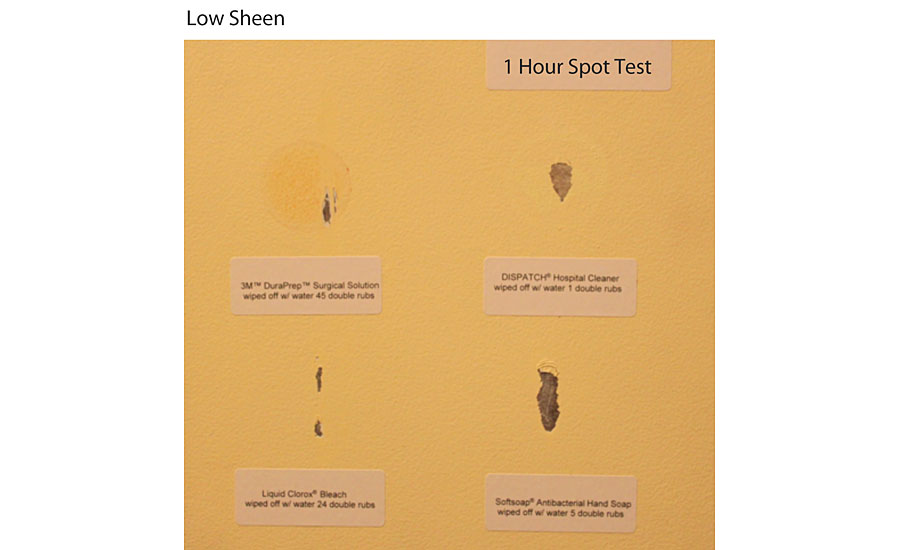
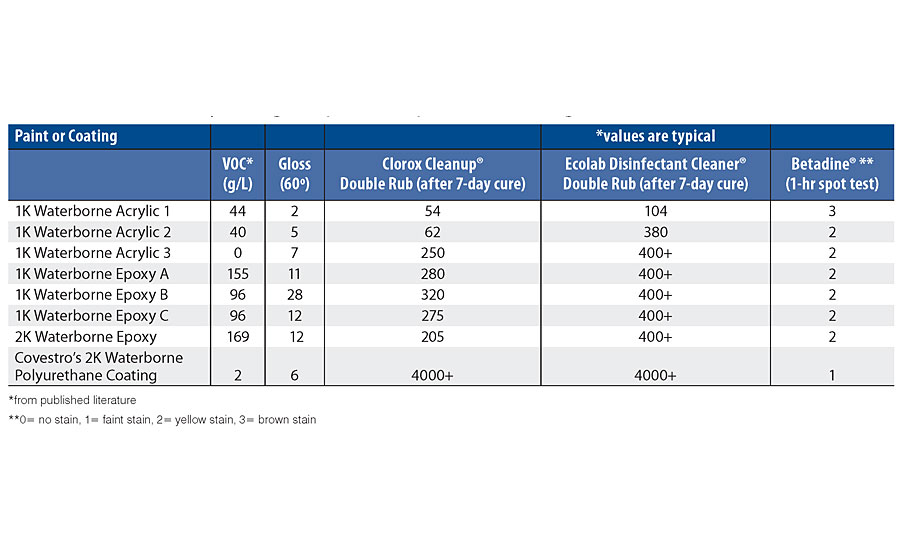
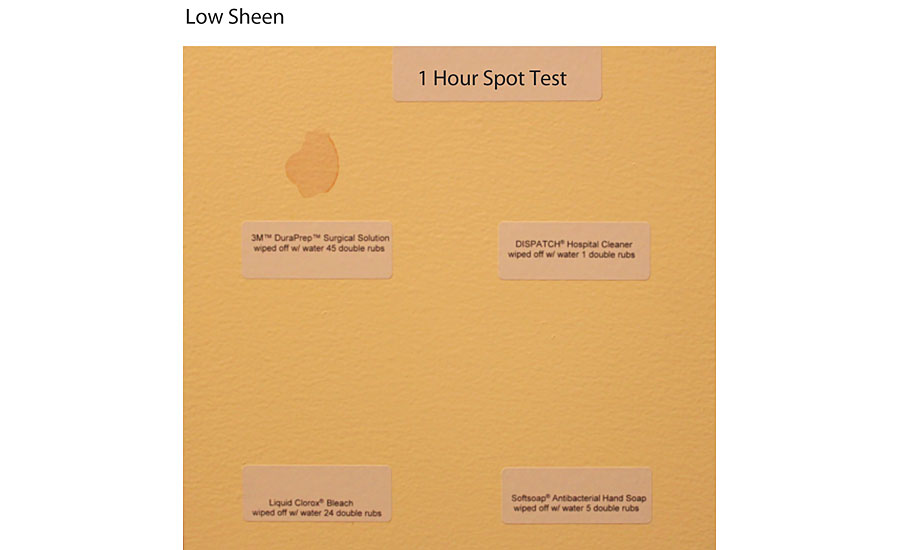
Wallboard panels were primed with a standard wall primer, coated with the test paints and coatings, and aged for 7 days to eliminate cure time effects. Then, several scrubbability tests using common disinfection chemicals were performed to determine the durability of the finishes. These results are summarized in Table 3. Pictures of two of the tested samples for comparison are included in Figure 2 and Figure 3. It is important to note that the iodine-based Betadine ® product poses an additional issue for hospitals due to the strong staining potential. Although the Betadine left a stain on the surface of the 2K waterborne polyurethane coating, this stain was removed using a pre-wetted disposable wipe containing 10% sodium hypochlorite. The stain could not be removed from the corresponding acrylic paint using the same method, and resulted in failure in the paint film.
Odor Intensity and Characterization
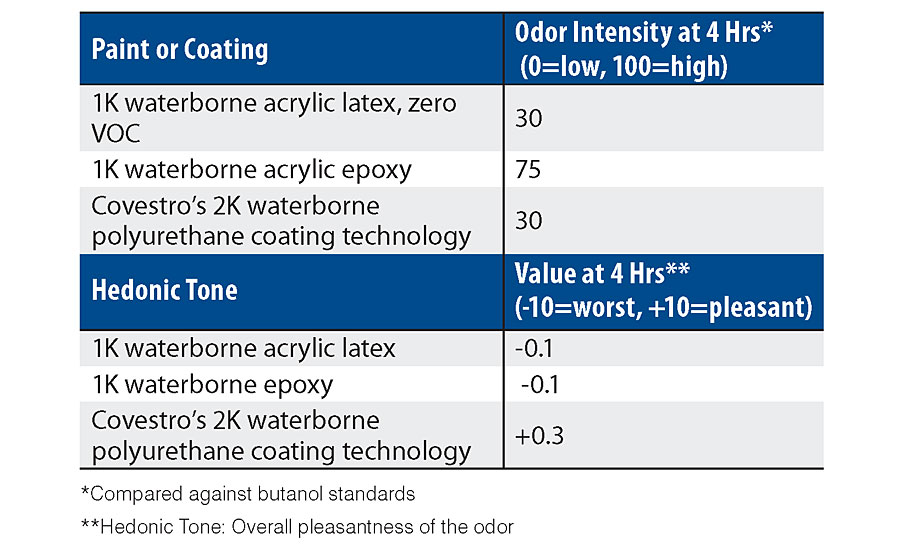
Since odor was a point of major concern for hospitals, a quantifiable odor test was performed by an independent sensory testing firm, St. Croix Sensory. This test compared the 2K waterborne polyurethane wall coating technology with several other acrylic and epoxy wall coatings that are recommended for the hospital environment. In both overall odor intensity and hedonic tones, the 2K waterborne polyurethane wall coating technology performed either equal to or better than the best performing alternative. For example, when the paint odor intensity was measured against butanol standards, the 2K waterborne polyurethane wall coating technology was equal to a lower performance acrylic recommended for hospitals due to its ultra-low odor and zero VOC, and much lower than a waterborne acrylic epoxy. For the hedonic tone category, which determines the overall pleasantness of the odor given off by the test substrate, the 2K waterborne polyurethane wall coating technology performed better than the other coatings that were tested, and was the only coating that crossed into the positive side of the metric ratings. These results are reported in Table 4.
Evaluating if the Prescription Fixed the Pains
In the testing protocol shown in Tab. 3, the double rubs represent the durability and cleanability of the coatings. The 2K waterborne polyurethane wall coating technology outperforms the one-component (1K) waterborne acrylic, the 1K epoxies and the 2K epoxies for durability against cleaning with industry-standard products, such as a 10% bleach solution for use against SARS-CoV-2. 5 The durability against the Ecolab Disinfectant Cleaner ® of Acrylic 3, Epoxy A, Epoxy B, Epoxy C, 2K Epoxy and the 2K waterborne polyurethane wall coating technology is better than Acrylic 1 and Acrylic 2. The 2K waterborne polyurethane wall coating technology also has better resistance to staining from Betadine than both the acrylics and the epoxies. The odor test in Tab. 4 shows that the 2K waterborne polyurethane wall coating technology has the best overall odor acceptability, taking both intensity and characterization into consideration.
With odor, durability and cleanability of the coating as major pain points for hospital administrators, the results show that the 2K waterborne polyurethane wall coating technology provides the best overall properties to meet these requirements.
However, other desired attributes were discussed with the hospital facility decision makers, 6 including the ability to use lower-gloss coatings to impart a desired aesthetic quality to the room. This could be done with traditional paints, but the additives that are used to lower the gloss reduce the abrasion resistance and increase the dirt pick-up of the wall surface. Therefore, facility owners have had a preference for gloss or semi-gloss finishes, primarily for durability reasons. 7 As previously detailed, resins that are used in the 2K waterborne polyurethane wall coating technology inherently interact with light in the final coating to cause a lower gloss without the need for copious amounts of property-reducing matting additives.
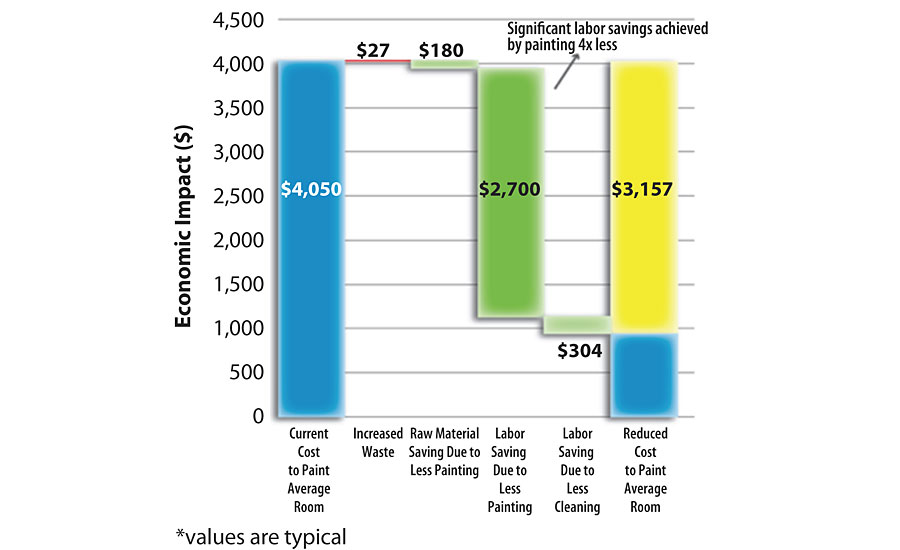
Another factor affecting the specification of a paint or coating, by architects with a fiduciary responsibility to their clients, is the total cost of maintenance. The total cost is a sum of labor and paint costs over a prescribed period of time. In the example summarized in Figure 4, a highly utilized set of operating rooms were painted roughly four times a year due to repeated cleaning with harsh disinfecting cleaners. In this economic waterfall, a typical applied cost was used for a waterborne acrylic paint based on multiple inputs from painting contractors, facility managers and environmental services personnel. Subsequent costs were listed as the comparison was made to switching several operating rooms over to the 2K waterborne polyurethane wall coating technology for five cycles. The additional cost in red was related to the fact that a 2K system cannot be mixed to the exact amount needed for one room. This waste quantity is dwarfed by the fourfold reduction in the amount of paint used based on the higher durability, allowing for a minimum of five times the longevity. The largest savings that were realized were based on the major reduction in labor costs as recorded in the fourth column. These reduced costs also support the facility owner’s desire to use the hospital’s own staff painters more. Finally, the hospital environmental services staff that was interviewed indicated a slight reduction in cleaning time due to the smooth surface of the 2K waterborne polyurethane wall coating technology as compared to other paints. This translates into the cost listed in the fifth column. Overall, the data shows that a coating based on the 2K waterborne polyurethane technologies exhibits an excellent cost/performance ratio, which alleviates some of the maintenance cost pains for a hospital administrator.
While these operational cost savings are for one high-risk room and are significant, it is important to understand the breadth of the healthcare assets that might benefit from these savings. A myopic portion of these assets can be gleaned from published survey data. For example, the American Hospital Association (AHA) conducts an annual survey of U.S. hospitals. The data from the fiscal year 2018 AHA Annual Survey indicates there are 6,146 U.S. hospitals housing roughly 98,000 intensive care rooms that are deemed critical due to multiple reasons, including exposure of mucous membranes or non-intact skin. These conditions increase the chance for HAIs and require specific disinfection and sterilization criteria. The study does not take into account the additional high-risk areas in these hospitals, such as emergency and operating rooms. 8 Additionally, the study does not account for outpatient facilities, urgent care facilities and primary care physician offices that would operate under the same disinfection guidelines.
The Prognosis Going Forward
The COVID-19 pandemic has escalated the aggressiveness and frequency of cleaning in higher-risk healthcare environments. This, coupled with existing guidelines, has created a need for more durable and chemical-resistant solutions in the healthcare built environment. 2K waterborne polyurethane architectural wall coating technology combines several desired performance properties that address pains identified by architects, facility managers and design professionals. Namely, this technology combines a very low VOC and low odor level with extremely high durability as measured by chemical and abrasion resistance. This unique combination of properties is very well-suited for healthcare environments where low odor and high performance are favored. The use of this 2K waterborne polyurethane technology offers the coating formulator options for creating a coating that significantly reduces the amount of repaint cycles and offers lower sheen without sacrificing durability or increasing dirt pick-up.
References
1 Patient Care Link, https://patientcarelink.org/improving-patient-care/healthcare-acquired-infections-hais, 2020.
2 Centers for Disease Control and Prevention, “Guideline for Disinfection and Sterilization in Healthcare Facilities”, Atlanta, GA. Centers for Disease Control and Prevention, 2008.
3 Interviews with multiple architects, facility managers, and consultants in the U.S., 2012-2020.
4 Reinstadtler, S.R. Environmentally Friendly Graffiti Resistant Coatings, SSPC Conference, February 2010.
5 https://www.cdc.gov/infectioncontrol/guidelines/disinfection/disinfection-methods/chemical.html.
6 Reinstadtler, S.R. New Architectural Coatings Technology Targeted At Stricter Hospital Infection Protocols, SSPC PACE Show, February 2012.
7 Reinstadtler, S.R. High Performance Wall Coatings Targeted at Stricter Hospital Infection Protocols, AIA Conference, June 2018.
8 2018 AHA Annual Survey Fast Facts, American Hospital Association, https://www.aha.org/statistics/fast-facts-us-hospitals.
Looking for a reprint of this article?
From high-res PDFs to custom plaques, order your copy today!